How historical disease tuberculosis spreads & who's at risk
Tuberculosis is often seen as a threat of the past. But it remains a significant concern worldwide, with international travel spreading the disease.
While tuberculous is rare in Australia, and we no longer routinely vaccinate against it, clusters of cases in South Australia over the past 17 months have put health authorities on alert.
So what exactly is tuberculosis, how is it treated and what is Australia doing to prevent its transmission?
It starts as a respiratory infection
Tuberculosis, caused by the bacterium Mycobacterium tuberculosis, starts as a respiratory infection when inhaled.
Once in the lungs, the immune system responds by forming granulomas, clusters of immune cells (mainly macrophages and T cells), in an attempt to contain the infection.
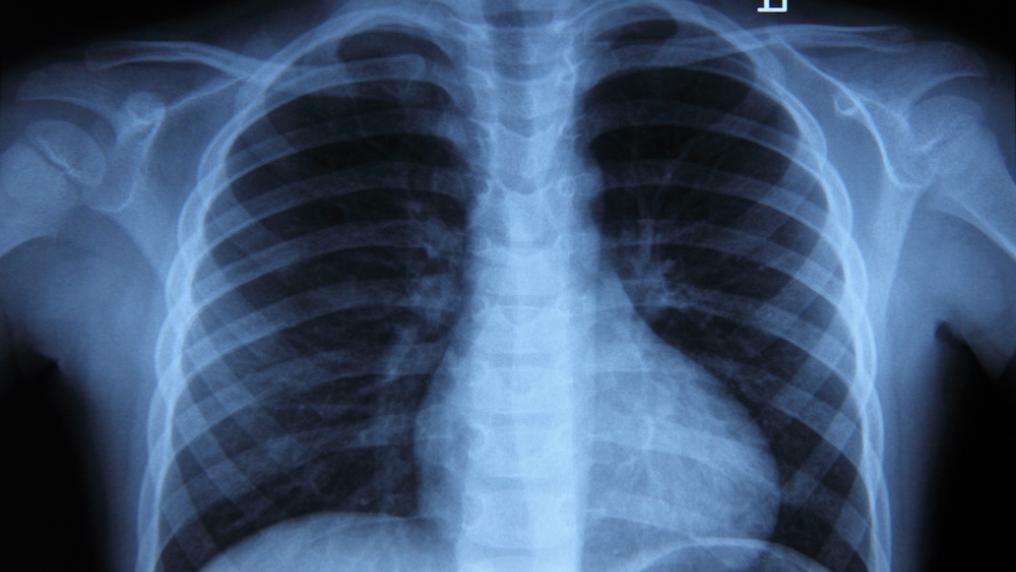
Over time, some granulomas may calcify, with calcium salts accumulating within these structures.
These calcifications are visible on X-rays and indicate latent tuberculosis infection. This means the Mycobacterium tuberculosis are in a dormant state, causing no immediate symptoms but posing a potential risk of reactivation if the host’s immune defences weaken.
Reactivation can lead to active tuberculosis, characterised by symptoms such as a persistent cough, fever, weight loss and fatigue.
Active tuberculosis is contagious, especially when it affects the lungs, as it primarily spreads through respiratory droplets released during coughing or sneezing.
Early treatment is key
Early diagnosis and treatment reduces the infectious period and helps prevent spreading the disease to others. It can also halt the progression of a latent infection to active disease.
Delayed treatment can lead to complications such as lung damage and scarring; damage to the bones, kidneys, lymph nodes and central nervous system; and infection in the brain and spinal cord. Delayed treatment can also be fatal.
Antibiotic treatment, often involving multiple drugs, is highly effective at eliminating the bacteria.
However, it can be lengthy, lasting several months or more. This can be physically and emotionally challenging for patients, especially as it includes periods of isolation.
Treating tuberculosis can also be a notable burden on the health system, due to the need for isolation, contact tracing, and specialised care.
Tackling drug-resistant bacteria
The Mycobacterium tuberculosis bacteria can quickly become resistant to antibiotics, so routine treatment includes multiple antibiotics which increases adverse effects.
The emergence of drug-resistant tuberculosis strains is a major concern because it makes treatment significantly more challenging and costly. Managing drug-resistant tuberculosis often requires extended treatment courses with second-line drugs, which can lead to more severe side effects and demand close monitoring.
Drug-resistant tuberculosis strains are also associated with higher rates of death.
The prolonged and complex treatment regimens increase the risk of treatment non-compliance and failure, posing not only a threat to affected people but also raising concerns about potential community transmission of these drug-resistant strains.
Who is susceptible to tuberculosis?
The risk of acquiring tuberculosis is higher among people who live in densely populated housing, those with compromised immune systems and people with poor access to health care.
This includes Indigenous Australians, recent migrants and refugees, people with underlying health conditions (such as HIV or diabetes), people in corrections facilities, remote and rural communities, the elderly, and people who are homeless, as well as health-care workers.
Children are also at greater risk of tuberculosis, as their immune systems are still developing.
Tuberculosis often presents differently in children, making it challenging to estimate the true global burden. However, the World Health Organization estimates 11% of the 10.6 million tuberculosis cases worldwide are in children. Some 14% of all tuberculosis-related deaths occur in children under 15 years old.
Common symptoms of paediatric tuberculosis include prolonged cough, wheezing, weight loss, loss of appetite, respiratory symptoms, failure to thrive, swelling of the lymph nodes, fever and night sweats.
Infants are also at increased risk of:
- disseminated tuberculosis. This spreads throughout the body via the bloodstream and lymphatic system to the liver, spleen, bone marrow, kidneys and brain
- tuberculous meningitis. This is a life-threatening condition where the infection from the lungs has gone to the brain and spinal cord
- congenital tuberculosis. This is a rare condition where a newborn baby is born with active tuberculosis, transmitted from infected mother to baby.
What can we do about TB?
Despite Australia’s relatively low incidence of tuberculosis, we have a robust control program, targeting efforts to vulnerable populations through culturally sensitive health-care services, public health campaigns, and community engagement.
The Bacille Calmette-Guérin vaccine provides partial protection, primarily against severe forms of tuberculosis. It’s not routinely given in Australia because we’re not considered a high-risk country, but it’s given in local regions with tuberculosis outbreaks.
Active tuberculosis must be reported to health authorities in Australia. This is important to prevent spread of tuberculosis in the community.
Testing for active tuberculosis is also a part of the immigration process. Visa applicants aged 11 years and over must have a chest X-ray for evidence of active tuberculosis.
SA Health is working with Aboriginal Community Controlled Health Organisations and other partners to respond to this outbreak with information and videos.
Timely and effective tuberculosis control measures help not only in treating individuals but also in preventing further transmission. This reduces the overall impact of the disease on public health and the health-care system.
Dr Ena Husaric, a doctor at The Royal Children’s Hospital Melbourne, co-authored this article.
Vasso Apostolopoulos, Professor of Immunology, Vice-Chancellors Distinguished Professorial Fellow, Head of Immunology and Translational Research, Victoria University and Maja Husaric, Senior Lecturer; MD, Victoria University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
![]()



